Unit 12. Stree Prajanananga Nirmana and Vikruti Topic A: Development of the Female Reproductive System from the Müllerian Duct and Its Anomalies
Unit 12A: Development of the Female Reproductive System from the Müllerian Duct and Its Anomalies
Learning Goals
By the end of this lesson, you should be able to:
- trace the embryological development of the female tract from the Müllerian (paramesonephric) ducts,
- list the normal derivatives of the Müllerian system and structures not derived from it,
- explain how defects at specific steps (formation, fusion, canalisation, resorption, vertical fusion) lead to distinct anomalies,
- classify congenital uterine anomalies (CUA) using commonly used systems, and
- recognise key clinical features, imaging findings, reproductive implications and management principles for each anomaly.
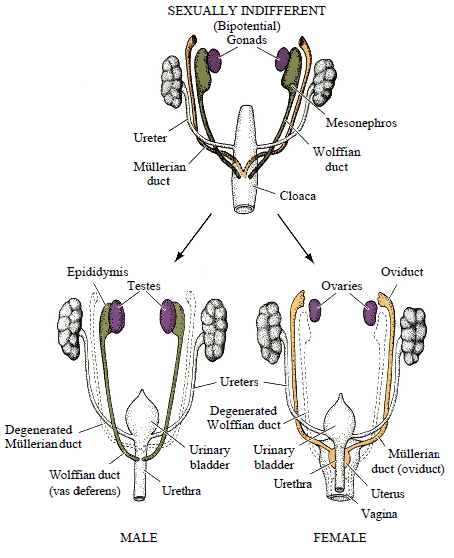
The female reproductive system develops from an indifferent embryo via Müllerian ducts in the absence of testosterone, forming the uterus, fallopian tubes, and vagina. Ovaries also differentiate from the gonadal ridges, producing eggs that are arrested until puberty. Puberty, triggered by the pituitary gland releasing hormones, stimulates the ovaries to produce estrogen, leading to sexual maturity and the start of the menstrual cycle with the release of eggs.
Embryological Development (Fetal Life)
- Initial Stage:The development begins around 6 weeks of gestation with two pairs of undifferentiated duct systems: the Wolffian ducts and the Müllerian ducts.
- Müllerian Duct Development:In the absence of male hormones (like testosterone), the Müllerian ducts develop and form the female reproductive organs.
- Organ Formation:The two Müllerian ducts grow, fuse in the midline, and develop into the uterus, fallopian tubes, and upper part of the vagina.
- Ovarian Development:The gonadal ridges develop into the ovaries, which start to form immature egg cells (oocytes).
Development in Adolescence (Puberty)
- Hormonal Trigger:The pituitary gland, located in the brain, begins to produce hormones that signal the ovaries to start making female sex hormones, especially estrogen.
- Sexual Maturation:The rise in estrogen levels causes the physical changes associated with sexual maturity.
- Menstrual Cycle:Near the end of puberty, the ovaries begin releasing eggs monthly through a process called the menstrual cycle. The first period is called menarche.
Key Factors and Considerations
- Hormonal Influence:The presence or absence of the male hormone testosterone is crucial for determining whether the reproductive system develops along male or female lines.
- Environmental Factors:Genetics, nutrition, and other environmental factors can influence the age at which puberty begins and the overall development of the system.
- Associated Structures:The female reproductive tract develops alongside the urinary tract and other organs, so developmental differences can sometimes affect these other areas as well.
1) Embryological Overview (Weeks 5–20)
- Embryonic origin: Intermediate mesoderm → urogenital ridge. Two paired ducts develop: mesonephric (Wolffian) and paramesonephric (Müllerian).
- Sex determination: In genetic females (46,XX), no Anti-Müllerian Hormone (AMH) is present; Müllerian ducts persist and differentiate. In males, Sertoli-cell AMH causes Müllerian regression.
- Timeline (approximate):
- Week 5–6: Coelomic epithelium invaginates lateral to mesonephros to form Müllerian ducts cranially open to the coelom (future fimbrial ostia).
- Week 7–9: Caudal migration medial to mesonephric ducts; crossing and midline fusion into a single uterovaginal primordium.
- Week 9–12: Canalisation of ducts begins; contact with urogenital sinus forms the Müllerian tubercle and induces sinovaginal bulbs.
- Week 12–20: Resorption of the midline septum within the fused portion → single endometrial cavity; vaginal plate canalises from cranial (Müllerian) and caudal (sinovaginal) components; hymen remains as a thin membrane.
Molecular patterning
- WNT4: essential for Müllerian development and ovarian differentiation; loss can cause Müllerian aplasia with virilisation.
- HOXA genes: segmental identity—HOXA10 (uterine body), HOXA11 (lower uterine segment/cervix), HOXA13 (upper vagina).
- PAX2, LHX1 (LIM1): early duct formation and maintenance.
Understanding these explains why defects can be region-specific.
2) What the Müllerian Ducts Form—and What They Do Not
| Structure | Embryological source |
|---|---|
| Fallopian tubes (oviducts) | Unfused cranial Müllerian ducts (infundibulum, ampulla, isthmus) |
| Uterus (garbhāśaya) | Fused Müllerian ducts (uterovaginal primordium); myometrium from surrounding mesenchyme |
| Cervix | Caudal part of fused Müllerian ducts |
| Upper 2/3 of vagina (yoni-mārga) | Müllerian contribution (uterovaginal primordium) |
| Lower 1/3 of vagina + hymen | Urogenital sinus (endoderm) via sinovaginal bulbs and vaginal plate |
| Ovaries | NOT Müllerian: arise from gonadal ridge (mesenchyme) with primordial germ cells |
| External genitalia (labia, clitoris) | NOT Müllerian: from genital tubercle/folds (ectoderm & mesenchyme) |
High-yield point: Ovaries and lower vagina are not Müllerian; this explains why some anomalies present with a normal ovary and external genitalia but absent uterus/upper vagina.
3) Step-by-Step Normal Development
- Initiation and elongation: Coelomic epithelium invaginates to form paired Müllerian ducts that grow caudally alongside mesonephric ducts.
- Cranial patency: Cranial ends remain open to the coelomic cavity → future fimbrial ostia.
- Midline fusion: Caudal ends fuse to form the uterovaginal canal.
- Canalisation: Lumen forms within each duct and within the fused canal.
- Septal resorption: The midline septum between the fused ducts is resorbed to create a single uterine cavity and cervix.
- Vertical fusion: The uterovaginal canal meets the urogenital sinus at the Müllerian tubercle; sinovaginal bulbs form a vaginal plate which later canalises, leaving the hymen.
Defect at any step → predictable anomaly, reviewed below.
4) Congenital Anomalies: Concepts and Pathogenesis
Congenital Müllerian anomalies (also called congenital uterine anomalies, CUA) occur in ~4–7% of the general population, with higher prevalence among women with infertility, recurrent pregnancy loss, or adverse obstetric outcomes. Renal tract anomalies co-exist in up to 20–30%, due to shared embryological origin—hence the need to image kidneys whenever a Müllerian anomaly is identified.
Grouping by the stage that fails
- Formation (agenesis/hypoplasia): Partial or complete absence of Müllerian derivatives—e.g., MRKH (Mayer–Rokitansky–Küster–Hauser) syndrome: absent/ rudimentary uterus and upper vagina, normal ovaries/karyotype (46,XX).
- Fusion defects (lateral fusion): Failure of ducts to fuse → uterus didelphys (double uteri/cervices ± longitudinal vaginal septum), or bicornuate uterus (partial fusion failure, heart-shaped fundus).
- Canalisation defects: Poor lumen formation—may cause transverse vaginal septum.
- Resorption defects (septal resorption): Persistence of a midline septum → septate uterus (complete or partial septum).
- Vertical fusion defects: Failed junction between Müllerian cranial vagina and sinus-derived caudal vagina → imperforate hymen, transverse vaginal septum (functional outflow obstruction).
- Dysmorphic uterine cavity: e.g., T-shaped uterus classically linked to in-utero diethylstilbestrol (DES) exposure (rare today); may also be idiopathic.
5) Common Classification Systems
(A) ASRM/AFS (classic)
- Class I: Hypoplasia/Agenesis (e.g., MRKH)
- Class II: Unicornuate uterus (± rudimentary horn)
- Class III: Uterus didelphys
- Class IV: Bicornuate uterus
- Class V: Septate uterus
- Class VI: Arcuate uterus (mild indentation; often considered a normal variant)
- Class VII: DES-related anomalies (T-shaped)
(B) ESHRE/ESGE (2013; widely cited)
- U0: Normal uterus (includes minor variants)
- U1: Dysmorphic uterus (e.g., T-shaped)
- U2: Septate uterus
- U3: Bicorporeal uterus (bicornuate spectrum)
- U4: Hemi-uterus (unicornuate)
- U5: Aplastic uterus (± rudimentary cavity)
- U6: Unclassified
Exam tip: Know both schemes and be able to map common entities.
6) Distinguishing Key Anomalies (Diagnosis and Imaging)
Preferred imaging: 3D transvaginal ultrasound (3D-TVS) and MRI (gold standard in complex cases). Hysterosalpingography (HSG) shows the internal cavity but not the fundal contour; laparoscopy directly assesses the external fundus and may be combined with hysteroscopy for diagnosis + treatment.
Septate vs Bicornuate vs Didelphys
| Feature | Septate uterus | Bicornuate uterus | Uterus didelphys |
|---|---|---|---|
| Embryological error | Failure of septal resorption | Partial fusion failure | Complete fusion failure |
| External fundal contour | Normal/flat or shallow indentation | Deep fundal cleft (external indentation) | Two separate hemi-uteri with deep fundal cleft |
| Cervix | Usually single | Usually single (bicornuate unicollis) or double (bicornuate bicollis) | Double cervix |
| Vagina | Usually single | Often single | Often longitudinal vaginal septum present |
| Diagnosis key | Normal fundal contour on MRI/3D-TVS with internal septum | External fundal indentation; intercornual distance widened | Two distinct uteri and cervices; “double” appearance |
| Management | Hysteroscopic septal resection | Selected cases: Strassman metroplasty (rare, for adverse obstetric history) | Usually no unification surgery; resect obstructing vaginal septum if present |
7) Major Anomalies—Clinical, Imaging, Management
7.1 MRKH (Müllerian agenesis; Class I / U5)
- Anatomy: Absent/ rudimentary uterus; absent upper vagina; normal ovaries, normal secondary sexual characteristics, 46,XX.
- Presentation: Primary amenorrhoea with normal thelarche and adrenarche; sometimes renal (agenesis, ectopia) or skeletal anomalies.
- Investigations: MRI pelvis; abdominal/renal ultrasound.
- Management: Non-surgical vaginal dilation (first-line) or vaginoplasty (McIndoe, Vecchietti) when needed; reproductive options include gestational surrogacy or uterus transplant (select centres). Psychological support essential.
7.2 Unicornuate uterus (Class II / U4)
- Pathogenesis: Agenesis of one duct → hemi-uterus; may have a rudimentary horn (with or without cavity, communicating or non-communicating).
- Risks: Infertility, miscarriage, preterm birth, malpresentation; rudimentary horn pregnancy (life-threatening rupture).
- Management: Surgical excision of a non-communicating functional rudimentary horn; high-risk antenatal surveillance in pregnancy.
7.3 Uterus didelphys (Class III / typically U3 if both corpora fully separate)
- Anatomy: Two separate uteri and cervices; frequently a longitudinal vaginal septum (dyspareunia, obstructive symptoms if asymmetric).
- Outcomes: Often reasonable fertility; increased miscarriage/preterm risk.
- Management: Usually conservative; resect an obstructive vaginal septum. Unification surgery rarely indicated.
7.4 Bicornuate uterus (Class IV / U3—bicorporeal)
- Anatomy: Single cervix (unicollis) or double cervix (bicollis) with deep external fundal cleft.
- Obstetric issues: Miscarriage, preterm birth, malpresentation.
- Management: Conservative; in women with recurrent pregnancy loss or extreme preterm births attributable to the anomaly, metroplasty (Strassman) may be considered in selected centres. Cervical cerclage may be needed based on history/cervical length.
7.5 Septate uterus (Class V / U2)
- Anatomy: Normal external fundus; internal septum (fibromuscular) dividing the cavity—complete to the external os or partial (subseptate).
- Reproductive impact: Highest rate of first-trimester miscarriage among uterine anomalies; infertility association debated but often considered significant.
- Management: Hysteroscopic septal resection improves live-birth rates and reduces miscarriage.
7.6 Arcuate uterus (Class VI; normal variant in many schemas)
- Anatomy: Mild concavity at the fundus; not associated with significant adverse outcomes.
- Management: No treatment.
7.7 DES-related / T-shaped uterus (Class VII / U1 dysmorphic)
- Anatomy: Narrowed, T-shaped cavity; hypoplastic cervix. Today, most T-shaped cavities are idiopathic.
- Presentation: Infertility, recurrent loss, poor implantation.
- Management: Hysteroscopic metroplasty (lateral wall incisions) in selected symptomatic cases.
7.8 Transverse vaginal septum (vertical fusion/canalisation defect)
- Site: Upper, mid or lower vagina.
- Presentation: Primary amenorrhoea with cyclical pain (haematocolpos/haematometra), dyspareunia, obstructed labour.
- Treatment: Surgical resection with careful mucosal anastomosis; postoperative dilators to maintain patency.
7.9 Imperforate hymen (vertical fusion remnant)
- Presentation: Adolescents with primary amenorrhoea, cyclical pain, bulging bluish membrane, urinary retention.
- Treatment: Cruciate incision hymenotomy and drainage under asepsis.
8) Clinical Clues, Complications and Co-morbidities
- Amenorrhoea + normal secondary sexual characteristics → think MRKH or outflow obstruction (imperforate hymen, transverse septum).
- Cyclical pain after menarche without bleeding → outflow obstruction (non-communicating horn with endometrium, imperforate hymen).
- Infertility/recurrent loss → consider septate or bicornuate uterus; differentiate with imaging.
- Pregnancy complications: miscarriage (especially septate), preterm labour, malpresentation, IUGR in severe anomalies.
- Associated anomalies: Renal (agenesis, duplication), skeletal (vertebral, limb). Always screen kidneys.
9) Investigation Strategy
- Baseline pelvic ultrasound (2D → 3D reconstruction if available).
- MRI pelvis when diagnosis is uncertain or complex; best for fundal contour, cervical anatomy, rudimentary horn characterisation, and associated renal anomalies.
- HSG for cavity outline and tubal patency (pre-surgery infertility workup), noting it cannot define the external fundus.
- Diagnostic hysteroscopy ± laparoscopy: when intervention is planned (e.g., septal resection) or differentiation remains unclear.
- Renal ultrasound in every confirmed Müllerian anomaly.
10) Management Principles
- Correct only what is clinically relevant. Not all anomalies require surgery.
- Septate uterus: hysteroscopic resection (safe, effective).
- Non-communicating rudimentary horn with functional endometrium: laparoscopic excision to prevent endometriosis and rupture.
- Obstructive vaginal anomalies (transverse septum/imperforate hymen): timely relief with meticulous technique; maintain patency with dilators.
- Bicornuate/didelphys: major unification surgeries are rare; consider only for severe obstetric morbidity after multidisciplinary review.
- MRKH: staged dilation programmes first; surgery only when indicated; psychosocial support; discuss fertility options.
- Antenatal care: high-risk surveillance—cervical length monitoring, consider cerclage for proven cervical insufficiency, manage malpresentation (version/LSCS as indicated).
11) Ayurveda Correlation (for integrative understanding)
Classical texts describe the formation of the yoni-mārga and garbhāśaya as part of śarīra development, emphasising the coordinated contribution of maternal and paternal factors, diet (ahara), conduct (vihāra), and daivavyapāśraya. While the modern embryological steps above explain exact morphogenesis, the clinical emphasis on preserving patency (āvaraṇa-nivṛtti), preventing retained blood (rakta sanga), and ensuring healthy conception and gestation parallels the classical aims of garbhāsaṁskāra, ṛtumati paricaryā, and prasava-saṃrakṣaṇa. (Direct śloka quotation is not essential here because this is a modern embryology topic.)
12) Key Take-Home Points (Rapid Revision)
- Müllerian ducts form fallopian tubes, uterus, cervix and upper vagina; ovaries/external genitalia are not Müllerian.
- Defect mapping (formation, fusion, canalisation, resorption, vertical fusion) predicts the anomaly.
- Septate vs bicornuate hinges on external fundal contour (normal vs cleft).
- Always screen kidneys once a Müllerian anomaly is diagnosed.
- Septal resection is the commonest effective corrective procedure; major unification surgeries are uncommon today.
- Tailor management to symptoms, reproductive plans and obstetric history.
Assessment
A) MCQs (choose one best answer)
- Upper two-thirds of the vagina develops from:
A. Urogenital sinus B. Müllerian ducts C. Mesonephric ducts D. Cloaca
Answer: B. Rationale: Upper 2/3 is Müllerian; lower 1/3 is sinus-derived. - The anomaly with normal external fundus but internal division of the cavity is:
A. Bicornuate B. Didelphys C. Septate D. Unicornuate
Answer: C. Rationale: Septate = resorption failure with normal fundal contour. - A 16-year-old girl has primary amenorrhoea, normal breast/axillary hair, and a blind-ending short vagina. Most likely diagnosis:
A. Androgen insensitivity B. MRKH C. Turner syndrome D. Hypothalamic amenorrhoea
Answer: B. Rationale: MRKH: absent uterus/upper vagina with normal secondary sexual characters. - Non-communicating rudimentary horn is dangerous because of:
A. Cervical incompetence B. IUGR C. Horn pregnancy rupture D. Placenta accreta
Answer: C. - First-line imaging to differentiate septate from bicornuate uterus:
A. HSG B. 2D US only C. 3D-TVS or MRI D. CT scan
Answer: C. - Failure of lateral fusion of Müllerian ducts leads to:
A. Septate uterus B. Uterus didelphys C. Arcuate uterus D. T-shaped uterus
Answer: B. - A painful bulging intact hymen in an adolescent with amenorrhoea suggests:
A. Transverse septum B. Imperforate hymen C. MRKH D. Cervical atresia
Answer: B. - The congenital uterine anomaly most strongly linked with first-trimester miscarriage is:
A. Bicornuate B. Septate C. Didelphys D. Arcuate
Answer: B. - In MRKH, the ovaries are:
A. Absent B. Dysgenetic C. Normal and functional D. Virilised
Answer: C. - DES-related cavity shape classically is:
A. Heart-shaped B. T-shaped C. Banana-shaped D. Pear-shaped
Answer: B.
B) Short Answer Questions (write 3–5 lines each)
- Enumerate normal derivatives of the Müllerian ducts.
- Describe the embryological basis of a septate uterus.
- Differentiate uterus didelphys from bicornuate uterus (two points).
- Outline the evaluation of a patient with suspected MRKH.
- Why should renal imaging be done in Müllerian anomalies?
C) Long Answer Questions
- Describe the development of the female reproductive tract from the Müllerian ducts, including timing, molecular cues (WNT4, HOXA), and contributions from the urogenital sinus. Add a note on structures not derived from Müllerian ducts.
- Classify congenital Müllerian anomalies. Explain pathogenesis, clinical features, fertility/obstetric implications, diagnostic approach, and management of septate uterus and bicornuate uterus.
D) Case-Based (OSCE-style) Prompt
A 24-year-old woman with two first-trimester miscarriages undergoes HSG showing two endometrial cavities. Describe how you would differentiate septate vs bicornuate uterus, list the next best imaging, and state definitive management if septate uterus is confirmed.
Self-Check (2 minutes)
- Can you name five Müllerian anomalies and the developmental step that failed in each?
- Can you state one key imaging sign that distinguishes septate from bicornuate?
- Do you remember which part of the vagina is not Müllerian?
If yes, you are exam-ready for this topic.
